Alright lads let’s get into it. You’ve had testicular cancer. That’s no small thing and the fact you’re on the other side of it means you’re a fighter, a winner, and a legend in the game. This shouldn’t be glossed over, but in the interest of sticking to the point and not beating around the bush (every pun intended) let’s get straight to it.
Your surgery is done. Maybe you’ve had chemotherapy or radiotherapy during your treatment. Either way, you’ve been through the wringer, and now you’re probably wondering, “What’s the deal with sex now?”
The short answer: You can still have sex. Good sex. Great sex, even. Well…we can’t vouch for you in that respect, but it is possible! There may be a few things you need to navigate along the way, but that’s in the long answer, which you can find if you continue reading.
Back in the saddle – when can I get jiggy again?
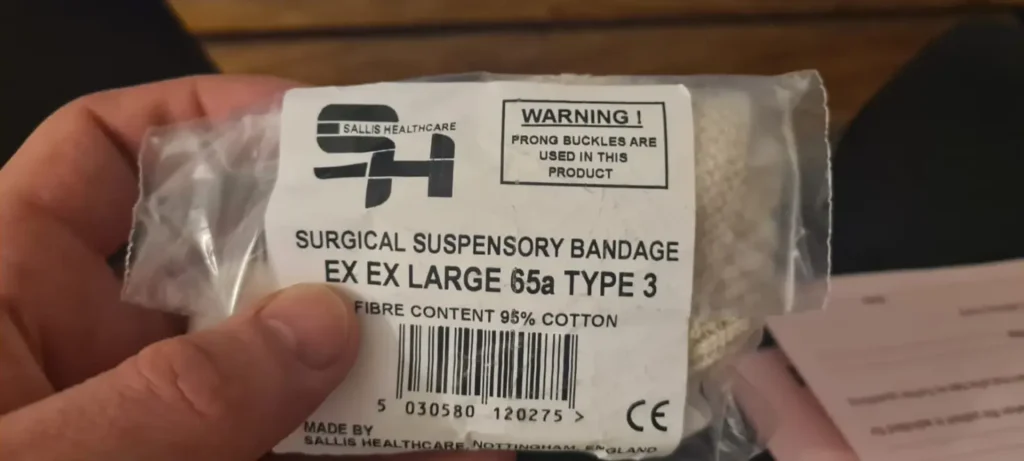
If you’ve had surgery to remove one testicle (orchiectomy) the general rule is once the stitches are out, the swelling’s down, and you’re not wincing when you sit — you’re probably good to go. That’s usually around 4 to 6 weeks following your surgery. Everyone is different though and you shouldn’t rush things! Even if you are keen to! You don’t want to have to explain an awkward ‘relapse’ to your doctor because you got overexcited.
If you have had both testicles removed it may change things a bit. This is because you will no longer be producing your own testosterone. Your sex drive, erections, and fertility might take a hit. But don’t panic, there are treatment options for that.
Testosterone and you
Even with one testicle you may experience low levels of testosterone, which may make you feel tired, moody, or just not up for sex. If that happens, have a word with your doctor. Testosterone replacement therapy is a thing, and it works a charm for lots of men in the UK.
Before any treatment starts, your medical team might offer you free sperm banking on the NHS. It’s like saving your swimmers for a rainy day, and it’s worth thinking about if you want kids later on in life.
Radiotherapy and chemotherapy concerns
Radiation and chemotherapy can cause a bit of a temporary buzzkill in the bedroom as some guys find their libido drops, or things don’t quite rise to the occasion. This is totally normal. Things should return back to how they used to be once your treatment is complete. Just give it time. It will be worth it! You may also be advised to use contraception for a short period of time following radiation treatment.
More than just motion in the ocean
The hardest part of bouncing back isn’t always the physical side of sex. It’s what’s going on in your head that can get in the way of a good time. Your confidence might take a knock or you might feel a bit different about your body. Maybe you don’t feel sexy, or you’re scared things won’t go the way they used to. That’s all legit and totally normal, and also nothing to be ashamed of admitting.
You’ve been through a big life change, one that affects you mentally enough as it is anyway. It comes with physical changes and anything that changes your appearance is bound to make you think inwardly about how you look.
Try this:
- Catch yourself when you’re talking or thinking negatively about your body — and counter it with something positive. Don’t be shy either. If you don’t bang your own drum no one will ever hear the sound of your beat!
- Remember you’re still you. One testicle down doesn’t change your worth, your desirability, or your swagger.
- Look after your body. Eat decent food, rest, and keep active. Physical health feeds into mental health, and vice versa.
Addressing the physical changes
In truth, once everything heals, there really isn’t that much difference in appearance. This is especially true if you opt for a prosthetic replacement. Honestly and truly, take this from a team of testicular cancer survivors, you cannot tell the difference in the cold light of day. Your scar will heal nicely and is around your abdominal area, much like a scar from having an operation on your appendix, so it is not obvious what the scar is from. And the prosthetic looks no different to a human testicle. Let’s be honest fellas (unless you’re really kinky) how much time does anyone spend down there examining it? Don’t answer that!
The performance chat
If you’ve ever referred to yourself as a ‘machine’ in bed — good news, you probably still are. So that’s us all then, right? Most guys don’t notice much difference in what their bodies can do. You might see a drop in the amount of semen when you climax, but we’re talking fractions here. Unless you’re measuring output by the pint, it’s really not worth stressing about.
Talking to your partner (or someone new)
Already got a partner? Talk to them. Be honest about what’s changed and what hasn’t. Tell them what feels good, what doesn’t, and ask the same back. You might be surprised by how supportive they are.
Seeing someone new? It’s your call how much to share and when. If it’s a serious connection, they’ll want to know the real you and that includes your story. If they’re weird about it then the relationship isn’t for you, simple as.
You’ve got this! But you’re also not alone!
Look, we know this stuff isn’t always easy to talk about. But don’t bottle it up. There’s loads of support out there and most of it is from blokes who’ve been exactly where you are.
We’ve got therapy sessions through our charity. Most of us at Baggy Trousers UK have had testicular cancer ourselves. We get it. Drop us a line any time at support@baggytrousersuk.org — no judgment, no nonsense, just real chat.
Prefer a group vibe? There are support groups too. Your treatment centre might run one, or your GP can point you in the right direction. It’s easy to focus on the physical healing and ignore what’s going on upstairs. But your emotional wellbeing matters just as much, especially when it comes to sex.
So take your time. Ask for help if you need it. Laugh when you can. Cry when you need to. And when the time’s right – get back in the game!